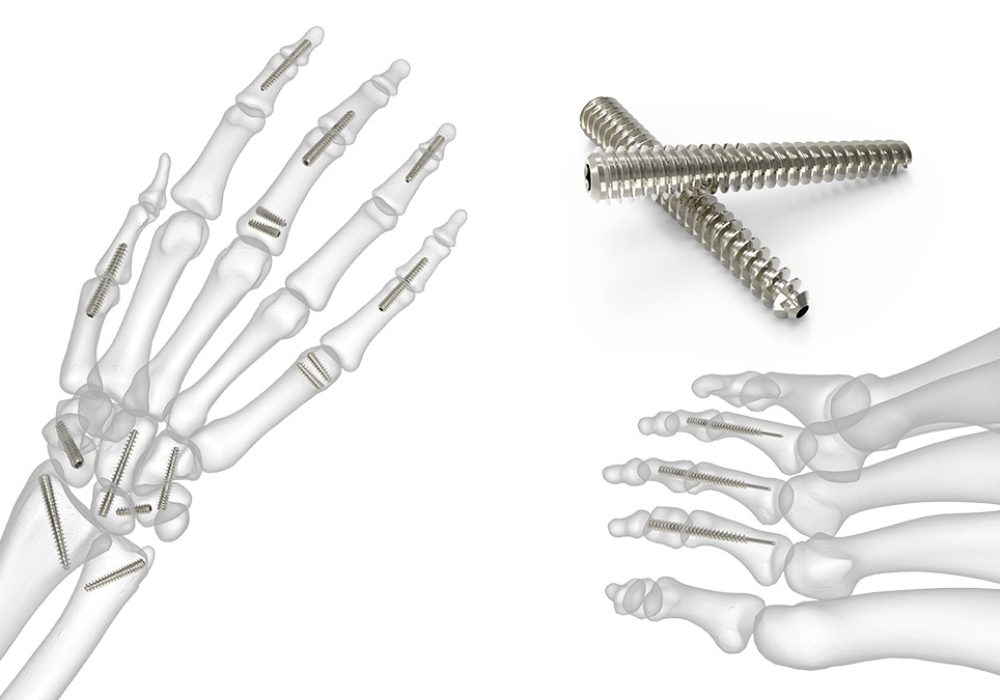
Headless screw fixation of carpus
Headless screw fixation of the carpus represents a significant advancement in the surgical management of carpal bone fractures and instability. This technique utilizes specialized screws designed to provide stable internal fixation while minimizing soft tissue irritation and preserving joint function. The carpus, composed of eight small bones arranged in two rows, plays a crucial role in wrist mobility and load transmission. Injuries to these bones, whether from trauma or degenerative conditions, often require precise and stable fixation to restore anatomy and function. Headless screws have become a preferred option due to their unique design and biomechanical advantages.
Anatomy and Biomechanics of the Carpus
Understanding the anatomy of the carpus is essential for effective fixation. The carpal bones include the scaphoid, lunate, triquetrum, pisiform, trapezium, trapezoid, capitate, and hamate. These bones form complex articulations that allow for the wrist’s wide range of motion, including flexion, extension, radial and ulnar deviation, and circumduction. The carpal bones are stabilized by a network of ligaments, and their blood supply is often tenuous, especially in the scaphoid, making fractures prone to nonunion or avascular necrosis.
The biomechanical environment of the carpus involves significant compressive and shear forces during wrist movement and load bearing. Therefore, fixation devices must provide sufficient stability to withstand these forces while allowing early mobilization to prevent stiffness and promote healing.
WRIST TREATMENTS
- Distal Radius Plating
- Percutaneous Scaphoid Screw
- Headless Screw Fixation of Carpus
- Dequervains Tenosynovitis Release
- Ganglion Cyst Removal
- Carpal Tunnel Release Surgery
- Mini Carpal Tunnel Release Surgery
- Open Carpal Tunnel Release Surgery
- Endoscopic Carpal Tunnel Release Surgery
- Scaphoid Nonunion Bone Grafting
- Scapholunate Ligament Reconstruction
- Proximal Row Carpectomy
- Arthroscopic TFCC Repair
- TFCC Reconstruction
- Limited Wrist Fusion Surgeries (SC fusion, RSL Fusion)
- Darrachs Procedure
- Wafers Resection of ulna
Make Your Appointment
Principles of Headless Screw Fixation
Headless screws are designed to be fully embedded within the bone, eliminating the protruding screw head that can irritate surrounding soft tissues or interfere with joint movement. These screws typically have a variable pitch thread, which allows for compression across the fracture site as the screw is advanced. The compression promotes bone healing by reducing micromotion and enhancing stability.
The screws are made from biocompatible materials such as titanium or stainless steel, which provide strength and resistance to corrosion. Their design often includes a tapered tip for easier insertion and self-tapping threads to reduce the need for pre-drilling in some cases.
Indications for Headless Screw Fixation in the Carpus
Headless screw fixation is primarily indicated for fractures of the carpal bones that require stable internal fixation. Common indications include:
- Scaphoid fractures: Particularly waist and proximal pole fractures, which are prone to nonunion due to limited blood supply.
- Capitate fractures: Rare but often associated with other carpal injuries.
- Lunate fractures: Less common but may benefit from stable fixation.
- Carpal instability: Certain ligamentous injuries or osteochondral fragments may be stabilized using headless screws.
- Nonunions and delayed unions: Revision surgeries where stable fixation is necessary to promote healing.
Surgical Technique
The surgical approach depends on the specific carpal bone involved and the fracture pattern. Generally, the procedure involves the following steps:
- Preoperative Planning: Imaging studies such as X-rays, CT scans, or MRI are used to assess fracture characteristics and plan screw placement.
- Exposure: A minimal incision is made to access the fracture site, preserving soft tissue and blood supply.
- Reduction: The fracture is anatomically reduced, often under fluoroscopic guidance.
- Guidewire Insertion: A guidewire is placed across the fracture to ensure correct trajectory.
- Drilling and Tapping: Depending on the screw design, drilling and tapping may be performed to prepare the bone.
- Screw Insertion: The headless compression screw is inserted over the guidewire, compressing the fracture fragments.
- Verification: Fluoroscopy confirms proper screw placement and fracture reduction.
- Closure: Soft tissues are closed carefully to minimize postoperative complications.
Advantages of Headless Screw Fixation
- Minimized Soft Tissue Irritation: The screw is buried within the bone, reducing the risk of tendon irritation or hardware prominence.
- Compression at Fracture Site: Variable pitch threads provide interfragmentary compression, promoting faster and more reliable healing.
- Preservation of Joint Motion: The absence of a screw head allows for smoother joint surfaces and less interference with wrist movement.
- Early Mobilization: Stable fixation permits early range of motion exercises, reducing stiffness and improving functional outcomes.
- Reduced Need for Hardware Removal: Because the screws are less likely to cause irritation, secondary surgeries for hardware removal are less common.
Clinical Outcomes and Complications
Clinical studies have demonstrated favorable outcomes with headless screw fixation in carpal fractures, particularly in scaphoid fractures where union rates exceed 90% in many series. Patients typically experience reduced pain, improved grip strength, and restoration of wrist function.
However, complications can occur, including:
- Nonunion or delayed union: Particularly in fractures with poor vascularity or inadequate fixation.
- Hardware failure: Screw breakage or loosening, though rare with modern designs.
- Infection: As with any surgical procedure, infection risk exists but is generally low.
- Tendon irritation or rupture: Though minimized, improper screw placement can still affect tendons.
- Avascular necrosis: Especially in proximal pole scaphoid fractures, despite fixation.
Postoperative Care and Rehabilitation
Postoperative management involves immobilization in a splint or cast for a variable period depending on fracture stability and healing progress. Early controlled mobilization is encouraged once sufficient healing is evident to prevent joint stiffness and muscle atrophy.
Physical therapy focuses on restoring range of motion, strength, and function. Regular follow-up with imaging ensures fracture healing and hardware integrity.
Innovations and Future Directions
Advances in imaging, surgical techniques, and implant design continue to improve outcomes in headless screw fixation of the carpus. Navigation systems and 3D printing assist in preoperative planning and custom implant design. Biodegradable screws and bioactive coatings are under investigation to enhance healing and reduce the need for hardware removal.
Minimally invasive approaches and arthroscopic-assisted fixation are gaining popularity, offering reduced soft tissue disruption and faster recovery.
Conclusion
Headless screw fixation of the carpus is a reliable and effective method for managing carpal fractures and instability. Its biomechanical advantages, combined with minimally invasive techniques, allow for stable fixation, early mobilization, and excellent functional recovery. Surgeons must carefully select patients and employ meticulous surgical technique to optimize outcomes and minimize complications. As technology evolves, headless screw fixation will likely remain a cornerstone in the treatment of complex carpal injuries.
Headless screw fixation of the carpus is an innovative and increasingly preferred technique for the treatment of carpal bone fractures and related wrist injuries. This method offers several biomechanical and clinical advantages over traditional fixation methods, providing stable internal fixation while minimizing soft tissue irritation and preserving wrist function. Below is a comprehensive overview of headless screw fixation of the carpus, covering anatomy, surgical principles, indications, technique, outcomes, and future directions.
