Scaphoid Nonunion Bone grafting
Scaphoid nonunion is a challenging condition that occurs when a fracture of the scaphoid bone in the wrist fails to heal properly within the expected timeframe. The scaphoid, one of the small carpal bones, plays a crucial role in wrist stability and motion. Due to its unique blood supply and anatomical position, fractures of the scaphoid are prone to complications such as delayed healing or nonunion. When nonunion occurs, it can lead to persistent pain, decreased wrist function, and eventually arthritis if left untreated. Bone grafting has become a cornerstone in the surgical management of scaphoid nonunion, aiming to promote bone healing, restore anatomy, and improve wrist function.
Understanding Scaphoid Nonunion
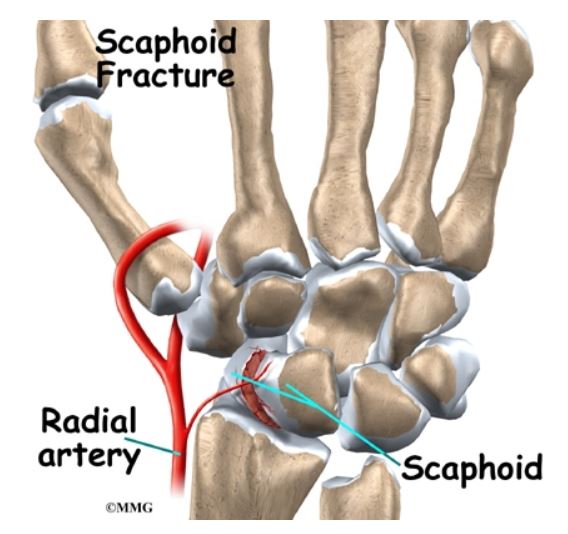
The scaphoid bone receives its blood supply primarily from branches of the radial artery, which enter distally and supply the proximal pole retrogradely. This vascular pattern makes the proximal fragment vulnerable to avascular necrosis (AVN) after fracture, especially in displaced or proximal pole fractures. Nonunion is defined as the failure of the fracture to heal after an adequate period, typically 6 months or more, and is often associated with persistent pain, tenderness in the anatomical snuffbox, and limited wrist motion.
Nonunion can be classified based on the presence or absence of AVN, the degree of bone resorption, and the presence of deformity such as the “humpback” deformity, where the scaphoid collapses and shortens, altering wrist biomechanics. These factors influence the choice of treatment and the type of bone grafting required.
Goals of Bone Grafting in Scaphoid Nonunion
The primary goals of bone grafting in scaphoid nonunion are to:
- Provide osteogenic cells and growth factors to stimulate bone healing.
- Restore the normal length and alignment of the scaphoid.
- Re-establish vascularity, especially in cases with AVN.
- Achieve stable fixation to allow early mobilization and prevent further displacement.
Bone grafting is often combined with internal fixation using screws or wires to stabilize the fracture and graft site.
WRIST PROBLEMS
- Distal Radius Fracture
- Distal Ulna Fracture
- Scaphoid Fracture, Nonunion
- Other Carpal Bone Fractures
- Dequervains Tenosynovitis
- Carpal Tunnel Syndrome
- Intersection Syndrome
- Swellings of Wrist Joint
- Ganglion Cyst
- Extensor Tenosynovitis
- Giant Cell Tumor of Distal Radius and Ulna
- Avascular Necrosis of Scaphoid
- Avascular Necrosis of Lunate (Keinbocks Disease)
- Distal RadioUlnar Joint & TFCC Injuries
- TFCC Tears (Acute & Chronic)
- DRUJ Instabilities & Dislocations
- Ulnocarpal Impaction Syndrome
- ECU Subluxation / ECU Tenosynovitis
- DISI (Dorsal Intercalated Carpal Instability)
- VISI (Volar Intercalated carpal Instability)
- SNAC Wrist (Scaphoid Nonunion Advanced Collapse)
- SLAC Wrist (Scapholunate Advanced Collapse)
- Lunate & Perilunate Dislocations
- Midcarpal Instabilities
- Radiocarpal Arthritis
- Mid-Carpal Arthritis
- Distal Radioulnar Joint Arthritis
Make Your Appointment
Types of Bone Grafts Used
Bone grafts used in scaphoid nonunion surgery can be broadly categorized into vascularized and non-vascularized grafts, as well as structural and non-structural grafts.
Non-Vascularized Bone Grafts
Non-vascularized bone grafts are harvested from sites such as the iliac crest or distal radius and transplanted to the nonunion site. These grafts provide osteoconductive scaffolding and osteogenic cells but rely on the recipient site for revascularization. They are typically used in cases without AVN and where the bone defect is small or moderate.
Advantages of non-vascularized grafts include relative technical simplicity and shorter operative time. However, their success depends on the local biological environment and the absence of significant bone necrosis.
Vascularized Bone Grafts
Vascularized bone grafts involve transplanting bone along with its blood supply, usually harvested from the distal radius or other donor sites with a known vascular pedicle. This technique is particularly beneficial in cases with AVN or large bone defects, as it provides immediate blood flow to the graft, enhancing healing potential.
Vascularized grafts are technically more demanding and require microsurgical expertise. Despite this, recent studies suggest that vascularized grafts do not always yield significantly superior outcomes compared to non-vascularized grafts in all cases, but they remain a valuable option for complex nonunions.
Structural vs. Non-Structural Grafts
Structural grafts are corticocancellous or cortical bone segments that provide mechanical support and help restore scaphoid length and shape. Non-structural grafts are cancellous bone chips that primarily serve to stimulate healing without providing significant mechanical strength.
The choice between structural and non-structural grafting depends on the degree of bone loss and deformity. Structural grafts are preferred when there is significant collapse or shortening of the scaphoid.
Surgical Techniques
The surgical approach to scaphoid nonunion with bone grafting typically involves open reduction, debridement of fibrous tissue and necrotic bone, bone graft placement, and internal fixation.
Exposure and Debridement: The nonunion site is exposed through a volar or dorsal approach depending on the location of the fracture and the presence of AVN. All fibrous tissue and sclerotic bone are removed to create a healthy bleeding bone bed.
Bone Graft Harvesting: The graft is harvested from the iliac crest, distal radius, or other donor sites. For vascularized grafts, the vascular pedicle is carefully preserved.
Graft Placement: The graft is shaped to fit the defect and restore the scaphoid’s normal anatomy. Structural grafts are used to correct deformity and maintain length.
Internal Fixation: Stable fixation is achieved using headless compression screws or Kirschner wires. This stability is critical for graft incorporation and fracture healing.
Postoperative Care: Immobilization in a cast or splint is maintained for several weeks, followed by gradual mobilization and rehabilitation.
Outcomes and Considerations
The success of bone grafting in scaphoid nonunion depends on multiple factors including the patient’s age, smoking status, duration of nonunion, presence of AVN, and surgical technique. Union rates reported in the literature vary but generally range from 80% to over 90% with appropriate treatment.
Non-vascularized grafting combined with stable fixation is effective in most cases without AVN or significant deformity. Vascularized grafts are reserved for more complex cases, such as proximal pole AVN or large bone defects, where enhanced blood supply is critical.
Complications can include persistent nonunion, donor site morbidity, infection, hardware failure, and stiffness. Early diagnosis and treatment improve outcomes, emphasizing the importance of timely intervention.
Advances and Future Directions
Recent research has focused on improving graft incorporation and healing through biological augmentation such as bone morphogenetic proteins (BMPs) and stem cell therapies. Minimally invasive techniques and arthroscopic-assisted bone grafting are also being explored to reduce surgical morbidity.
The debate between vascularized and non-vascularized grafting continues, with ongoing studies aiming to clarify indications and optimize patient selection. Personalized treatment plans based on imaging, vascular status, and biomechanical considerations are becoming the standard of care.
Conclusion
Bone grafting remains a fundamental component in the surgical management of scaphoid nonunion. Whether using vascularized or non-vascularized grafts, the goal is to restore the scaphoid’s anatomy, promote healing, and preserve wrist function. Careful patient evaluation, meticulous surgical technique, and appropriate postoperative management are essential to achieve successful outcomes and prevent long-term complications. As surgical techniques and biological therapies evolve, the prognosis for patients with scaphoid nonunion continues to improve, offering hope for full recovery and return to normal activities.
