Proximal Row Carpectomy
Proximal Row Carpectomy (PRC) is a surgical procedure performed to treat certain wrist conditions that cause pain, stiffness, and loss of function. It involves the removal of the proximal row of carpal bones—the scaphoid, lunate, and triquetrum—to relieve symptoms and preserve wrist motion. PRC is considered a motion-preserving salvage procedure and is often an alternative to wrist fusion in selected patients.
Anatomy of the Wrist and Proximal Carpal Row
The wrist is a complex joint composed of eight small carpal bones arranged in two rows: the proximal row and the distal row. The proximal row consists of the scaphoid, lunate, triquetrum, and pisiform bones. These bones articulate with the radius and ulna proximally and the distal carpal row distally, allowing for a wide range of wrist motion including flexion, extension, radial and ulnar deviation.
The proximal row plays a critical role in wrist stability and load transmission. However, when these bones are damaged due to trauma, arthritis, or avascular necrosis, they can become a source of pain and dysfunction.
Indications for Proximal Row Carpectomy
PRC is primarily indicated in patients with:
- Scaphoid nonunion advanced collapse (SNAC) wrist: A condition where a non-healed scaphoid fracture leads to progressive arthritis.
- Scapholunate advanced collapse (SLAC) wrist: Degenerative arthritis caused by chronic scapholunate ligament injury.
- Kienböck’s disease (stage II or III): Avascular necrosis of the lunate bone.
WRIST TREATMENTS
- Distal Radius Plating
- Percutaneous Scaphoid Screw
- Headless Screw Fixation of Carpus
- Dequervains Tenosynovitis Release
- Ganglion Cyst Removal
- Carpal Tunnel Release Surgery
- Mini Carpal Tunnel Release Surgery
- Open Carpal Tunnel Release Surgery
- Endoscopic Carpal Tunnel Release Surgery
- Scaphoid Nonunion Bone Grafting
- Scapholunate Ligament Reconstruction
- Proximal Row Carpectomy
- Arthroscopic TFCC Repair
- TFCC Reconstruction
- Limited Wrist Fusion Surgeries (SC fusion, RSL Fusion)
- Darrachs Procedure
- Wafers Resection of ulna
Make Your Appointment
- Post-traumatic arthritis: Following wrist fractures or ligament injuries.
- Failed previous wrist surgeries: When other treatments have not relieved symptoms.
Patients selected for PRC typically have preserved cartilage on the capitate and radius, as the procedure relies on the articulation between these two surfaces after removal of the proximal row.
Surgical Procedure
Preoperative Planning
Before surgery, detailed imaging studies such as X-rays, CT scans, or MRI are performed to assess the extent of arthritis and cartilage condition. The surgeon evaluates the integrity of the distal carpal row and the radius to ensure suitability for PRC.
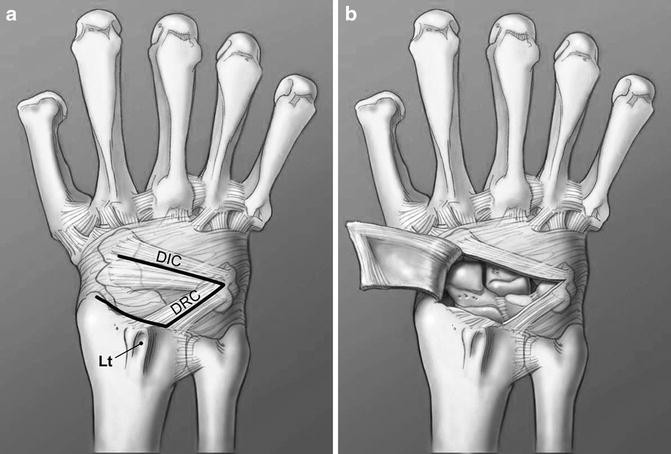
Operative Technique
Anesthesia and Positioning: The procedure is usually performed under general or regional anesthesia with the patient’s arm on an arm table.
Incision: A dorsal longitudinal or curvilinear incision is made over the wrist to expose the carpal bones.
Exposure: The extensor retinaculum and dorsal wrist capsule are carefully incised to access the proximal carpal row.
Removal of Proximal Row: The scaphoid, lunate, and triquetrum are excised en bloc. Care is taken to preserve the cartilage on the distal radius and capitate.
Assessment of Articulation: The surgeon inspects the capitate and radius surfaces to confirm they are suitable for articulation.
Closure: The capsule and retinaculum are repaired, and the skin is closed in layers.
Immobilization: The wrist is immobilized in a splint or cast postoperatively.
Postoperative Care and Rehabilitation
After surgery, the wrist is immobilized for approximately 4 to 6 weeks to allow soft tissue healing. Early motion exercises are then initiated under the guidance of a hand therapist to restore range of motion and strength.
Rehabilitation focuses on:
- Gradual wrist flexion and extension
- Forearm rotation exercises
- Grip strengthening
- Functional activities to improve dexterity
Patients typically regain a functional range of motion, although some loss compared to the normal wrist is expected.
Outcomes and Benefits
Proximal Row Carpectomy offers several advantages:
- Pain relief: Removal of arthritic bones reduces pain significantly.
- Preservation of motion: Unlike wrist fusion, PRC maintains partial wrist mobility.
- Improved function: Patients often return to daily activities and light work.
- Shorter recovery time: Compared to more complex reconstructive procedures.
Studies have shown that PRC provides good to excellent outcomes in carefully selected patients, with pain relief and functional improvement lasting for many years.
Limitations and Contraindications
PRC is not suitable for all patients. Contraindications include:
- Advanced arthritis involving the capitate or radius cartilage.
- Significant instability of the wrist.
- Severe deformity or collapse of the carpus.
- Patients requiring heavy manual labor or high-demand wrist use may not achieve optimal results.
In such cases, alternative procedures like partial wrist fusion or total wrist arthrodesis may be considered.
Potential Complications
As with any surgery, PRC carries risks, including:
- Infection
- Nerve injury
- Persistent pain or stiffness
- Progressive arthritis in the remaining wrist joint
- Instability or subluxation of the capitate
Close follow-up and adherence to rehabilitation protocols help minimize complications.
Comparison with Other Procedures
PRC is often compared with four-corner fusion (4CF), another motion-preserving salvage procedure. While 4CF fuses the capitate, lunate, hamate, and triquetrum bones, PRC removes the entire proximal row. PRC generally allows for greater wrist motion but may have a higher risk of progressive arthritis. The choice depends on patient factors, surgeon preference, and specific pathology.
Conclusion
Proximal Row Carpectomy is a valuable surgical option for patients with certain types of wrist arthritis and carpal bone pathology. By removing the diseased proximal carpal row, PRC alleviates pain while preserving wrist motion and function. Proper patient selection, meticulous surgical technique, and dedicated rehabilitation are essential for optimal outcomes. Patients considering PRC should discuss the benefits, risks, and alternatives with their orthopedic surgeon to make an informed decision.
