Primary Flexor tendon repair
Primary flexor tendon repair is a critical surgical procedure aimed at restoring hand function following injury to the flexor tendons. These tendons are responsible for bending the fingers and thumb, enabling gripping, grasping, and fine motor skills essential for daily activities. Injuries to the flexor tendons can severely impair hand function, and timely, effective repair is necessary to optimize recovery and minimize long-term disability.
Anatomy of Flexor Tendons
Tendon Surgery
Make Your Appointment
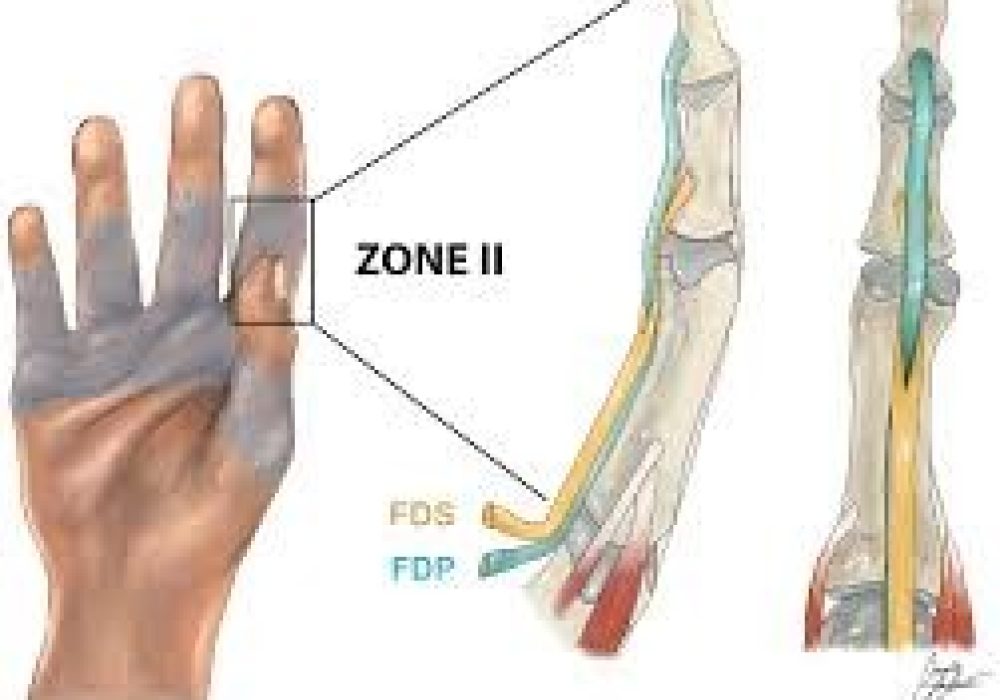
The flexor tendons are fibrous cords that connect the muscles of the forearm to the bones of the fingers and thumb. They run through a complex pulley system within the fingers, allowing smooth gliding and efficient finger flexion. The two main flexor tendons in each finger are:
- Flexor Digitorum Superficialis (FDS): Inserts on the middle phalanx and flexes the proximal interphalangeal (PIP) joint.
- Flexor Digitorum Profundus (FDP): Inserts on the distal phalanx and flexes the distal interphalangeal (DIP) joint.
The thumb has a single flexor tendon called the Flexor Pollicis Longus (FPL). These tendons are enclosed within a synovial sheath that provides nutrition and reduces friction during movement.
Mechanism of Injury
Flexor tendon injuries typically occur due to lacerations, crush injuries, or avulsions. Common causes include:
- Sharp cuts from knives, glass, or machinery.
- Sports injuries.
- Industrial accidents.
- Penetrating trauma.
Because the tendons lie close to the skin surface in the palm and fingers, they are vulnerable to injury. The injury may involve one or both tendons in a finger, and associated damage to nerves, blood vessels, or pulleys is common.
Zones of Flexor Tendon Injury
Flexor tendon injuries are classified into five anatomical zones, which guide treatment and prognosis:
- Zone I: From the fingertip to the insertion of the FDS tendon.
- Zone II: From the FDS insertion to the distal palmar crease (historically called “no man’s land” due to repair difficulty).
- Zone III: The palm area.
- Zone IV: The carpal tunnel.
- Zone V: The forearm.
Zone II injuries are particularly challenging because both FDS and FDP tendons run within a tight fibro-osseous sheath, making repair and rehabilitation complex.
Diagnosis
Diagnosis of flexor tendon injury involves:
- History and Physical Examination: Assessing the mechanism of injury, finger movement, and presence of lacerations.
- Functional Tests: Checking active flexion of the PIP and DIP joints to determine which tendons are injured.
- Imaging: Ultrasound or MRI may be used in complex cases to evaluate tendon integrity.
Prompt diagnosis is essential to plan surgical repair and prevent complications such as tendon retraction or adhesion formation.
Indications for Primary Flexor Tendon Repair
Primary repair is indicated when:
- The injury is fresh (usually within 1-2 weeks).
- The tendon ends are cleanly cut and can be approximated without tension.
- There is no significant contamination or infection.
- The patient is medically fit for surgery and able to comply with postoperative rehabilitation.
Delayed or secondary repair may be necessary if the injury is old or complicated by infection or scarring.
Surgical Techniques
The goal of primary flexor tendon repair is to restore tendon continuity with sufficient strength to allow early mobilization while minimizing bulk and interference with tendon gliding.
Preparation
- Surgery is usually performed under regional or general anesthesia.
- Tourniquet control is applied to provide a bloodless field.
- The wound is explored, and tendon ends are identified and debrided.
Repair Methods
Several suture techniques exist, with the choice depending on surgeon preference and injury characteristics. Common methods include:
- Modified Kessler Technique: A core suture technique using two strands crossing the repair site.
- Four-Strand Repair: Provides greater tensile strength by using four strands of suture material.
- Six-Strand or Eight-Strand Repairs: Used in some centers to allow early active motion protocols.
The core suture is usually supplemented with an epitendinous running suture to smooth the repair site and improve strength.
Suture Material
Non-absorbable, high-strength sutures such as polypropylene or polyester are preferred for core sutures. The epitendinous suture may use finer material to reduce bulk.
Pulley Management
Preservation of the annular pulleys (especially A2 and A4) is critical to maintain tendon biomechanics. If a pulley is damaged, it may be repaired or reconstructed.
Associated Injuries
Nerve or vessel injuries identified during surgery are repaired simultaneously to optimize functional recovery.
Postoperative Care and Rehabilitation
Successful outcomes depend heavily on meticulous postoperative management.
Immobilization
Initially, the hand is immobilized in a dorsal blocking splint with the wrist in slight flexion and the fingers in flexion to protect the repair.
Early Mobilization
Early controlled motion protocols are now standard to prevent adhesions and stiffness. These include:
- Passive Mobilization: The therapist moves the fingers within a safe range.
- Active Mobilization: The patient actively flexes and extends the fingers under supervision.
Protocols vary but generally start within the first week after surgery.
Monitoring
Regular follow-up is essential to monitor wound healing, tendon gliding, and detect complications such as rupture or infection.
Complications
Potential complications include:
- Tendon Rupture: Due to excessive tension or premature loading.
- Adhesions: Scar tissue limiting tendon gliding and finger motion.
- Infection: Particularly in contaminated wounds.
- Joint Stiffness: From prolonged immobilization or injury.
- Complex Regional Pain Syndrome (CRPS): A painful condition that can occur after hand surgery.
Outcomes
With modern surgical techniques and rehabilitation, primary flexor tendon repair can restore good to excellent function in most patients. Factors influencing outcomes include:
- Zone of injury (Zone II injuries are more challenging).
- Timing of repair.
- Patient compliance with therapy.
- Presence of associated injuries.
Early repair combined with supervised rehabilitation yields the best results, allowing patients to regain near-normal finger flexion and hand function.
Conclusion
Primary flexor tendon repair is a delicate but rewarding procedure that restores essential hand function after tendon injury. Understanding the anatomy, injury patterns, surgical techniques, and rehabilitation principles is vital for optimal outcomes. Advances in suture technology and early mobilization protocols continue to improve recovery, enabling patients to return to their daily activities and work with minimal disability.
