Microvascular Flaps: Advanced Techniques in Reconstructive Surgery
Microvascular flaps represent a revolutionary advancement in reconstructive surgery, enabling surgeons to repair complex defects by transferring tissue with its own blood supply from one part of the body to another. This technique involves microsurgical anastomosis of blood vessels, allowing free tissue transfer that can restore form and function in areas with significant tissue loss. This article provides an in-depth overview of microvascular flaps, including their types, surgical techniques, indications, benefits, and challenges.
What Are Microvascular Flaps?
Replantantation and Microsurgery
Make Your Appointment
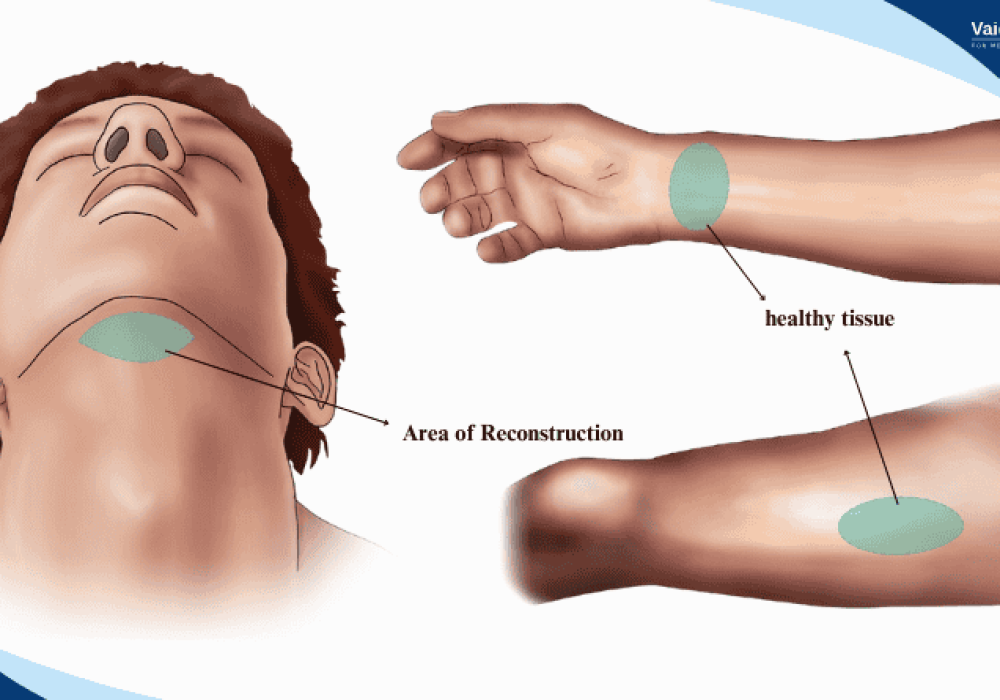
Microvascular flaps, also known as free flaps, are segments of tissue—comprising skin, muscle, bone, fat, or combinations thereof—that are completely detached from their original location and transplanted to a recipient site. The critical feature of microvascular flaps is the reconnection of the flap’s artery and vein to recipient vessels using microsurgical techniques under a microscope. This reestablishes blood flow, ensuring the survival of the transferred tissue.
This approach allows for the transfer of large and complex tissue volumes to distant sites, overcoming the limitations of pedicled or regional flaps.
Types of Microvascular Flaps
Microvascular flaps are classified based on the tissue components they contain:
1. Fasciocutaneous Flaps
These flaps include skin and underlying fascia, providing thin, pliable coverage ideal for resurfacing defects. Examples include:
- Radial forearm free flap
- Anterolateral thigh (ALT) flap
- Lateral arm flap
2. Muscle Flaps
Composed primarily of muscle tissue, these flaps are used to fill dead space, improve vascularity, and provide bulk. Examples:
- Latissimus dorsi free flap
- Gracilis free flap
- Rectus abdominis free flap
3. Osteocutaneous Flaps
These flaps include bone along with skin and soft tissue, used for reconstructing composite defects involving bone loss. Examples:
- Fibula free flap (commonly used for mandibular reconstruction)
- Scapular free flap
- Iliac crest free flap
4. Composite Flaps
These flaps combine multiple tissue types such as skin, muscle, bone, and nerve to address complex defects.
Indications for Microvascular Flaps
Microvascular free flaps are indicated in a wide range of reconstructive scenarios, including:
- Trauma: Reconstruction of extensive soft tissue and bony defects following accidents.
- Oncologic Surgery: Restoration of form and function after tumor resection, especially in the head and neck, breast, and extremities.
- Chronic Wounds and Infections: Coverage of non-healing wounds with well-vascularized tissue.
- Congenital Defects: Repair of complex congenital anomalies.
- Burn Reconstruction: Coverage of large burn defects where local tissue is insufficient.
The Microvascular Flap Procedure
The success of microvascular flap surgery depends on meticulous planning, surgical skill, and postoperative care. The procedure involves several key steps:
1. Preoperative Planning
- Detailed assessment of the defect and recipient site.
- Imaging studies such as Doppler ultrasound, CT angiography, or MRI to evaluate donor and recipient vessels.
- Selection of the appropriate flap based on tissue requirements and patient factors.
2. Flap Harvesting
- The flap is carefully dissected from the donor site, preserving the vascular pedicle (artery and vein).
- The length and caliber of vessels are optimized for anastomosis.
- The flap is completely detached from the donor site.
2. Flap Elevation
- Preoperative Assessment: Detailed evaluation including imaging studies, blood tests, and consultation with specialists such as vascular surgeons or oncologists.
- Surgical Planning: Determining the optimal level of amputation and planning for soft tissue coverage and nerve management.
- Amputation Surgery: The surgeon removes the affected portion of the arm, carefully managing blood vessels, muscles, and nerves to minimize pain and facilitate healing.
- Closure and Dressing: The surgical site is closed, often with a flap of healthy tissue to cover the bone end, and a sterile dressing is applied.
- Postoperative Care: Pain management, infection prevention, and monitoring for complications.
3. Recipient Site Preparation
- Recipient vessels are identified and prepared for microsurgical connection.
- The defect is debrided and prepared to receive the flap.
4. Microsurgical Anastomosis
- Using an operating microscope and microsurgical instruments, the surgeon connects the flap artery to the recipient artery and the flap vein to the recipient vein.
- Patency of the vessels is confirmed by observing blood flow.
5. Flap Inset and Closure
- The flap is positioned and sutured into the defect.
- Donor site closure is performed, sometimes requiring skin grafts.
6. Postoperative Monitoring
- Intensive monitoring of flap viability through clinical examination and adjunctive methods such as Doppler signals or implantable sensors.
- Early detection and management of vascular compromise are critical to flap survival.
Advantages of Microvascular Flaps
Microvascular free flaps offer several significant benefits:
- Versatility: Ability to transfer large and complex tissue volumes to distant sites.
- Improved Functional Outcomes: Restoration of form and function in challenging defects.
- Aesthetic Benefits: Better contour and color match with surrounding tissues.
- Multiple Tissue Types: Composite flaps allow simultaneous reconstruction of skin, muscle, bone, and nerve.
- Preservation of Local Tissue: Avoids sacrificing local or regional tissue that may be needed for future procedures.
Challenges and Risks
Despite their advantages, microvascular flaps present certain challenges:
- Technical Complexity: Requires specialized microsurgical training and equipment.
- Longer Operative Time: Procedures can be lengthy, increasing anesthesia risks.
- Flap Failure: Vascular thrombosis can lead to partial or complete flap loss.
- Donor Site Morbidity: Harvesting tissue can cause functional or cosmetic deficits.
- Cost: Higher resource utilization compared to simpler flap techniques.
Commonly Used Microvascular Flaps
Radial Forearm Free Flap
A thin, pliable fasciocutaneous flap based on the radial artery, commonly used for head and neck reconstruction. It offers reliable vascularity and ease of harvest but may cause donor site morbidity.
Anterolateral Thigh (ALT) Flap
A versatile fasciocutaneous or musculocutaneous flap based on the descending branch of the lateral circumflex femoral artery. It provides a large skin paddle with minimal donor site morbidity.
Fibula Free Flap
An osteocutaneous flap that includes a segment of fibula bone with overlying skin, ideal for mandibular and long bone reconstruction. It allows for dental implant placement and functional restoration.
Latissimus Dorsi Free Flap
A large muscle flap with or without skin, based on the thoracodorsal vessels, used for breast, chest wall, and extremity reconstruction.
Postoperative Care and Rehabilitation
Successful outcomes depend on vigilant postoperative care:
- Flap Monitoring: Regular assessment of color, temperature, capillary refill, and Doppler signals.
- Anticoagulation: Use of medications to prevent thrombosis as indicated.
- Physical Therapy: Early mobilization and rehabilitation to restore function.
- Psychological Support: Addressing emotional and psychological adaptation to reconstruction.
Future Directions in Microvascular Surgery
Advances continue to enhance microvascular flap surgery:
- Supermicrosurgery: Anastomosis of vessels less than 0.8 mm in diameter, expanding reconstructive possibilities.
- Perforator Flaps: Harvesting flaps based on small perforating vessels, minimizing donor site morbidity.
- Tissue Engineering: Combining flaps with bioengineered tissues for improved outcomes.
- Robotic-Assisted Microsurgery: Enhancing precision and reducing surgeon fatigue.
Conclusion
Microvascular flaps have transformed reconstructive surgery by enabling the transfer of complex tissue composites to restore form and function in challenging defects. While technically demanding, these procedures offer unparalleled versatility and outcomes when performed by skilled surgical teams. With ongoing innovations and multidisciplinary care, microvascular flap surgery continues to improve the lives of patients facing significant tissue loss due to trauma, cancer, or congenital conditions.
