Re-Implantation of amputated fingers, Hand & Upperlimb
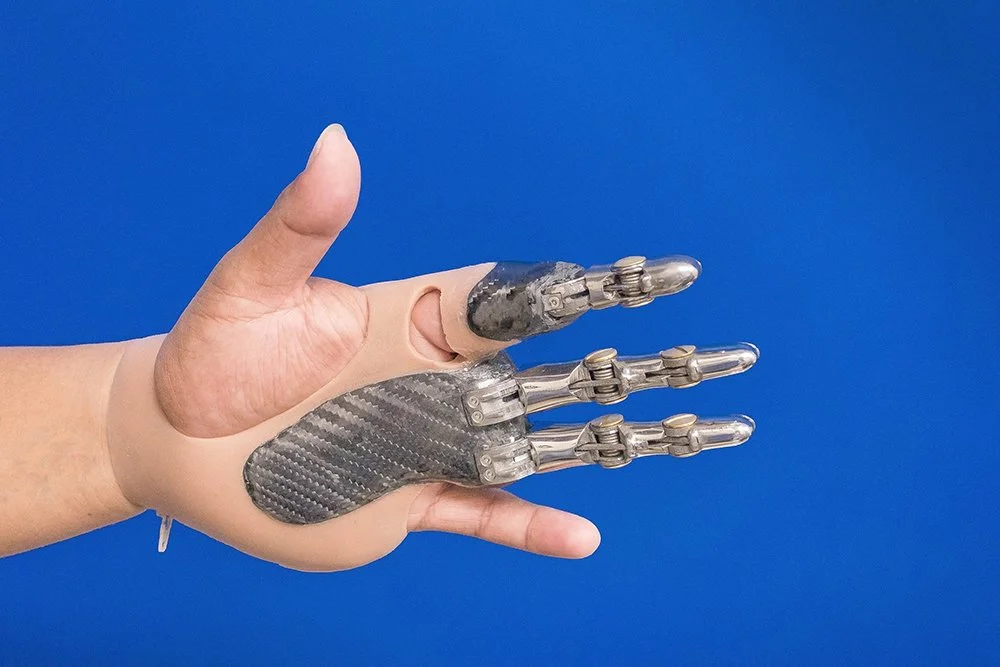
The re-implantation of amputated fingers, hand, and upper limb represents one of the most remarkable achievements in reconstructive microsurgery. This complex surgical procedure involves the reattachment of a completely severed body part, restoring both form and function. Advances in microsurgical techniques, anesthesia, and postoperative care have significantly improved the success rates and functional outcomes of these challenging surgeries.
Microsurgery
Make Your Appointment
Understanding Amputation and Re-Implantation
Amputation refers to the traumatic or surgical removal of a body part, such as a finger, hand, or part of the upper limb. Traumatic amputations often occur due to industrial accidents, road traffic collisions, or crush injuries. The loss of a finger or hand can have profound physical, psychological, and social impacts on a patient, affecting their ability to perform daily activities and work.
Re-implantation is the surgical reattachment of the amputated part to the remaining limb. It requires meticulous repair of bones, tendons, muscles, nerves, arteries, and veins under a microscope. The goal is to restore blood flow, sensation, and motor function to the amputated segment.
Indications for Re-Implantation
Not all amputations are suitable for re-implantation. The decision depends on several factors:
- Level of Amputation: Distal amputations (e.g., fingertip) are generally easier to re-implant than proximal amputations (e.g., forearm or upper arm).
- Condition of the Amputated Part: The amputated segment must be preserved properly (cool and clean) and free from severe crush or avulsion injuries.
- Patient’s General Health: Patients must be medically stable to undergo a lengthy microsurgical procedure.
- Time Since Amputation: Ideally, re-implantation should be performed within 6 to 12 hours of injury to maximize tissue viability.
- Functional Importance: Re-implantation is prioritized for thumbs and multiple finger amputations due to their critical role in hand function.
Preoperative Management
Proper preoperative care is essential for successful re-implantation:
- Preservation of the Amputated Part: The amputated finger or limb should be wrapped in sterile gauze, placed in a sealed plastic bag, and kept on ice. Direct contact with ice or water should be avoided to prevent frostbite.
- Assessment and Stabilization: The patient’s overall condition must be stabilized, including control of bleeding, pain management, and tetanus prophylaxis.
- Imaging: X-rays of the amputated part and stump help assess bone injury and plan fixation.
- Informed Consent: Patients should be counseled about the risks, benefits, and possible outcomes of re-implantation.
Surgical Technique
Re-implantation surgery is a multi-step process that requires a skilled microsurgical team:
1. Debridement and Preparation
Both the amputated part and the stump are carefully debrided to remove nonviable tissue while preserving as much healthy tissue as possible.
2. Bone Fixation
The first step in reconstruction is stabilizing the skeletal framework. This is usually done with Kirschner wires (K-wires), plates, or screws to align the bones properly.
3. Tendon Repair
Tendons controlling finger and wrist movement are repaired next. This step is crucial for restoring active motion.
4. Vascular Anastomosis
Microsurgical techniques are used to reconnect arteries and veins, restoring blood flow to the amputated part. This step is critical and often determines the success of the re-implantation.
5. Nerve Repair
Digital nerves are repaired to restore sensation. Although nerve regeneration is slow, early repair improves the chances of functional recovery.
6. Skin Closure
The skin is closed carefully to cover the repaired structures without tension.
Postoperative Care
Postoperative management is vital to ensure the survival of the re-implanted part and optimize functional recovery:
- Monitoring Circulation: The re-implanted finger or limb is closely monitored for signs of adequate blood flow, such as color, temperature, capillary refill, and bleeding on pinprick.
- Anticoagulation: Medications like heparin may be used to prevent blood clots in the repaired vessels.
- Immobilization: The limb is immobilized to protect the repair.
- Pain Management: Adequate analgesia is provided.
- Physical Therapy: Early and guided rehabilitation helps restore motion, strength, and function.
- Infection Prevention: Antibiotics and wound care reduce the risk of infection.
Functional Outcomes and Challenges
The success of re-implantation is measured not only by survival of the amputated part but also by the restoration of function. Outcomes vary depending on the level of amputation, patient age, and injury severity.
- Sensory Recovery: Sensory nerves regenerate at approximately 1 mm per day. Protective sensation usually returns within months, but fine discriminatory sensation may take longer or be incomplete.
- Motor Function: Tendon and muscle repair allow active movement, but stiffness and contractures are common challenges.
- Cosmetic Appearance: While re-implantation restores the limb’s appearance, scarring and deformities may occur.
- Psychological Impact: Successful re-implantation can significantly improve a patient’s quality of life and self-esteem.
Despite advances, some cases may require secondary procedures such as tendon transfers, nerve grafts, or corrective osteotomies to improve function.
Advances in Re-Implantation Surgery
Recent developments have enhanced the success and scope of re-implantation:
- Supermicrosurgery: Techniques allowing repair of very small vessels (<0.8 mm) have expanded the possibilities for distal fingertip re-implantations.
- Composite Tissue Allotransplantation: In cases where re-implantation is not possible, hand transplantation from donors is an emerging option.
- Tissue Engineering: Research into nerve regeneration and vascularized composite tissue engineering holds promise for future improvements.
- Improved Imaging: High-resolution imaging aids in preoperative planning and intraoperative navigation.
Conclusion
Re-implantation of amputated fingers, hand, and upper limb is a complex but highly rewarding surgical procedure that can restore form and function after devastating injuries. Success depends on timely intervention, meticulous surgical technique, and comprehensive postoperative care. With ongoing advances in microsurgery and rehabilitation, patients have better chances than ever before to regain meaningful use of their hands and upper limbs, improving their independence and quality of life.
