Opponensplasty: Overview, Indications, Procedure, and Recovery
Opponensplasty is a specialized surgical procedure designed to restore thumb opposition—the movement that allows the thumb to touch the fingertips, enabling grasp and fine motor skills. This surgery is particularly important for patients with median nerve palsy or other conditions that impair thumb function. By transferring a functioning tendon to the thumb, opponensplasty helps restore hand dexterity and improves the ability to perform daily activities.
Tendon Surgery
Make Your Appointment
What Is Opponensplasty?
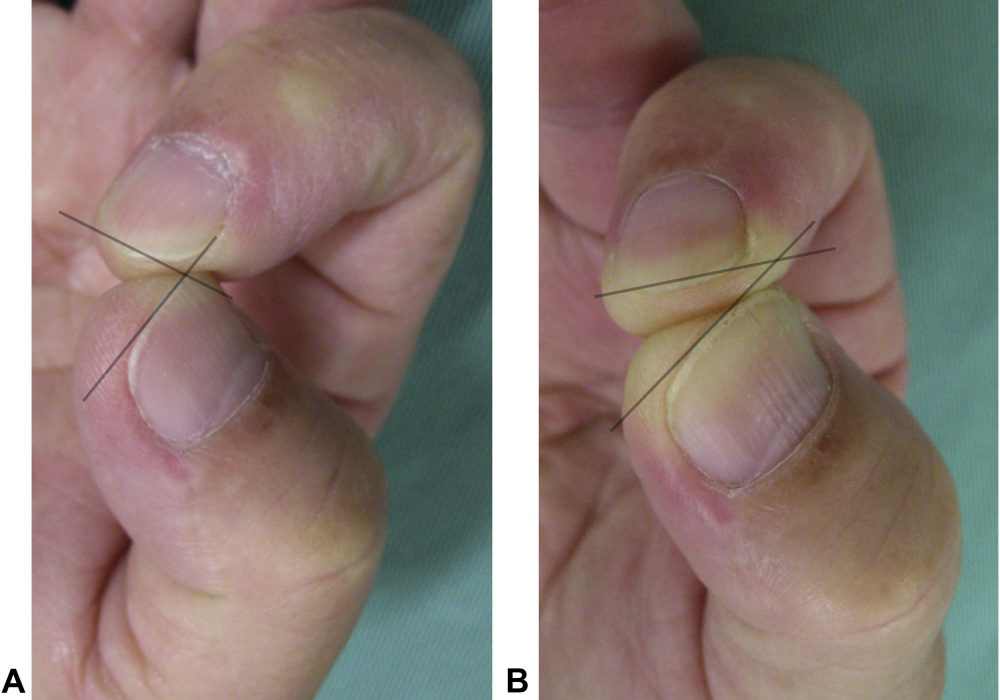
Opponensplasty involves transferring a tendon from a functioning muscle to replace the action of the paralyzed opponens pollicis muscle, which is responsible for thumb opposition. The procedure reestablishes the thumb’s ability to oppose the fingers, a critical movement for grasping, pinching, and manipulating objects.
Indications for Opponensplasty
Opponensplasty is indicated in patients with:
- Median nerve palsy: Resulting from trauma, compression (e.g., carpal tunnel syndrome), or birth injuries.
- Congenital hypoplasia or absence of the thenar muscles.
- Traumatic loss or paralysis of the opponens pollicis muscle.
- Failed nerve repair or nerve transfer surgeries affecting thumb opposition.
- Neuromuscular disorders causing intrinsic muscle weakness.
Goals of Opponensplasty
- Restore thumb opposition and abduction.
- Improve grip strength and hand function.
- Enhance fine motor skills.
- Prevent deformities such as thumb adduction contracture.
- Improve overall hand dexterity and quality of life.
Preoperative Evaluation
- Detailed clinical examination assessing thumb and hand function.
- Electromyography (EMG) to evaluate muscle activity.
- Imaging studies if needed to assess tendon and muscle status.
- Functional assessment to select the most suitable donor tendon.
Common Tendon Donors for Opponensplasty
- Flexor digitorum superficialis (FDS) tendon transfer: Most commonly used, typically from the ring finger.
- Palmaris longus tendon transfer: Used if present and suitable.
- Extensor indicis proprius (EIP) tendon transfer: Alternative donor in some cases.
- Abductor digiti minimi transfer: Less common.
The Opponensplasty Procedure
Surgical Steps
- Anesthesia: General or regional anesthesia is administered.
- Incision: Incisions are made to harvest the donor tendon and expose the thumb.
- Tendon Harvesting: The selected donor tendon is carefully detached while preserving its blood supply.
- Tendon Routing: The tendon is tunneled subcutaneously to the thumb.
- Attachment: The tendon is attached to the thumb’s metacarpal or the base of the proximal phalanx to recreate opposition.
- Tensioning: Proper tension is applied to allow effective thumb movement.
- Closure: Incisions are closed, and the hand is immobilized.
Duration
- The surgery typically lasts 1 to 2 hours.
Postoperative Care
- Immobilization in a splint or cast for 3 to 6 weeks.
- Pain management and wound care.
- Monitoring for complications such as infection or tendon rupture.
Rehabilitation and Recovery
- Physical and occupational therapy begin after immobilization.
- Exercises focus on restoring thumb opposition, strength, and coordination.
- Gradual return to functional activities.
- Full recovery may take several months.
Risks and Complications
- Infection
- Donor site weakness or functional loss
- Tendon rupture or failure
- Scar sensitivity or cosmetic concerns
- Incomplete restoration of thumb opposition
Prognosis
- Most patients experience significant improvement in thumb function.
- Success depends on careful patient selection, surgical technique, and rehabilitation.
- Early intervention and adherence to therapy optimize outcomes.
When to See a Doctor
Seek medical advice if you experience:
- Loss of thumb opposition or weakness.
- Difficulty with grasping or fine motor tasks.
- Pain, swelling, or signs of infection after surgery.
- Limited progress during rehabilitation.
Conclusion
Opponensplasty is a valuable surgical option for restoring thumb opposition and improving hand function in patients with median nerve palsy or intrinsic muscle paralysis. By transferring a functioning tendon, this procedure enables patients to regain essential hand movements necessary for daily living. Early evaluation by a hand surgeon and dedicated rehabilitation are key to achieving the best results. If you or your child has impaired thumb function, consult a specialist to explore whether opponensplasty is appropriate.
